You take that first step out of bed in the morning, and a sharp, stabbing pain shoots through your heel. It’s a familiar, dreaded start to the day. You limp to the bathroom, hoping it eases up as you move. Maybe you’ve tried rolling your foot on a frozen water bottle, stretching your calves against the wall, or buying expensive inserts for your shoes.
For a while, it feels a little better. But just when you think you’ve turned a corner, the pain returns—sometimes worse than before.
If this sounds like your daily reality, you are likely dealing with plantar fasciitis. It is one of the most common causes of heel pain we see here in South Jersey, but it is also one of the most misunderstood. The frustration often stems from a simple fact: standard advice like "just rest and stretch" rarely fixes the root of the problem.
At Optimal Health, we frequently see patients across South Jersey, who’ve tried everything from ice and orthotics to new shoes and daily stretching, yet still wake up with that familiar sharp heel pain.
So why doesn’t plantar fasciitis always heal with rest alone?
What Plantar Fasciitis Really Is
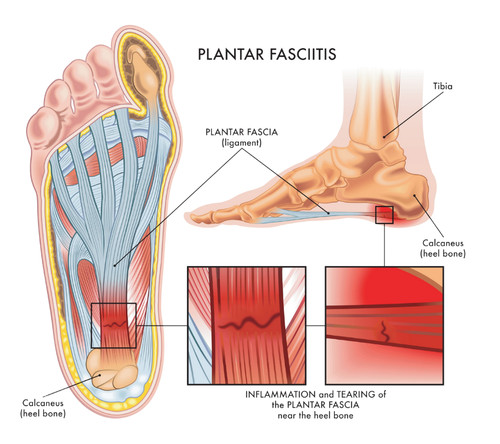
Plantar fasciitis involves irritation of the plantar fascia—a thick band of connective tissue that runs along the bottom of your foot, supporting your arch and absorbing force as you walk or run.
In the early stages, the condition may involve inflammation. However, when symptoms linger for weeks or months, the issue often becomes less about inflammation and more about poor tissue healing and overload. At this stage, rest and stretching may temporarily reduce discomfort, but they don’t always address why the tissue isn’t recovering.
Why Plantar Fasciitis Becomes Persistent
To understand why your heel pain won’t go away, it helps to look at what is actually happening inside your foot. The plantar fascia is a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. It acts like a shock absorber, supporting the arch of your foot as you walk or run.
When people first develop heel pain, it is often inflammation—the body’s initial response to injury. However, in cases where the pain lingers for months, the condition often changes. It shifts from an acute inflammatory issue (fasciitis) to a degenerative condition known as fasciosis.

In this chronic stage, the collagen fibers that make up the tissue begin to break down and become disorganized. Because the plantar fascia has a relatively poor blood supply compared to muscles, it struggles to repair this damage on its own.
Several factors contribute to this stalled healing process:
- Repetitive Strain: Every step you take places load on the tissue. If the tissue is weakened, normal walking can re-injure it before it has a chance to fully heal.
- Poor Load Tolerance: If the muscles in your foot and calf aren’t strong enough to handle the demands of your daily life, the plantar fascia takes on too much stress.
- Limited Blood Flow: As mentioned, tendons and thick connective tissues don’t get the same rich blood supply as muscles, making the repair process slower and more difficult.
Why Rest and Stretching Often Fall Short
It seems logical: if your foot hurts, stay off it. And if it feels tight, stretch it. While these strategies can offer short-term symptom relief, they often fail to provide a long-term cure.
The Problem with Rest:
Rest reduces the load on the tissue, which naturally reduces pain. But rest also weakens the tissue. When you eventually return to your normal activities—walking the dog, running, or standing at work—your plantar fascia is actually less capable of handling the stress than it was before. This cycle of "rest-weaken-reinjure" is a major reason symptoms keep coming back.
The Limitation of Stretching:
Stretching can feel good, but you cannot simply stretch away a tissue injury. In fact, aggressively stretching an irritated plantar fascia can sometimes aggravate it further. True healing requires the tissue to become more robust and capable of bearing weight, not just longer or looser.
How Shockwave Therapy Can Jumpstart Healing
For stubborn cases of plantar fasciitis that haven't responded to traditional care, we offer a non-invasive option at Optimal Health called Shockwave Therapy.
Despite the intense-sounding name, Shockwave Therapy (or Extracorporeal Shockwave Therapy) is a safe, evidence-based treatment that uses acoustic sound waves to target the damaged tissue. It does not involve electrical shocks.

Here is how it works to support healing:
- Stimulates Repair: The sound waves create "micro-trauma" in the tissue, which signals the body to restart its natural healing process. This is especially helpful for chronic conditions where the healing process has stalled.
- Increases Blood Flow: The treatment encourages the formation of new blood vessels (neovascularization) in the area, bringing essential nutrients and oxygen to the damaged tissue.
- Reduces Pain: Shockwave therapy can also help desensitize the nerve endings in the area, providing pain relief that allows you to move more comfortably during your recovery.
WATCH DR. PAUL TREATING PATIENT'S PLANTAR FASCIITIS WITH SHOCKWAVE: Watch here.
It is a powerful tool in our toolbox, often helping patients who thought surgery was their only remaining option.
A Comprehensive Approach to Foot Pain
While technologies like Shockwave Therapy are fantastic, they work best when combined with a holistic approach to movement. We don’t just treat the pain; we treat the person attached to the foot.
At our South Jersey clinics, we build a customized plan that may include:
1. Strengthening the Foot and Kinetic Chain
A strong foot is a resilient foot. We focus on strengthening the intrinsic muscles of the foot, as well as the calf, hamstring, and hip muscles. Often, weakness higher up the leg forces the foot to work overtime. By strengthening the entire chain, we take the pressure off your plantar fascia.
2. Manual Therapy and Joint Mobilization
Stiff ankles or restricted joints in the mid-foot can change the way you walk, placing uneven stress on your heel. Our physical therapists and chiropractors use hands-on techniques to mobilize these joints, ensuring your foot moves correctly with every step.
3. Gait and Movement Assessment
Sometimes the problem isn’t your foot—it’s how you walk. We analyze your gait to see if you are over-striding, landing heavily on your heel, or rolling your foot inward excessively. Small tweaks to your movement patterns can make a massive difference in reducing strain.
4. Load Management
We help you find the "Goldilocks zone" of activity—doing enough to stimulate healing without doing so much that you re-injure the tissue. This isn't about complete rest; it's about modifying your activity so you can stay active while you heal.
When to Seek Professional Guidance
If heel pain has lasted more than a few weeks, keeps returning, or limits your ability to stay active, it may be time to look beyond rest and stretching alone. Persistent pain often signals that the tissue needs more structured support to heal properly.
If you’re dealing with ongoing plantar fasciitis, the team at Optimal Health is here to help you understand what’s driving your pain and explore treatment options focused on long-term relief—not just quick fixes.





